Settle in, because this is going to be a long story. Or just skip this entirely if birth stories aren't your thing! Even before I got pregnant I was fascinated by birth stories - probably because I watched A Baby Story all the time when I was in college! But I know they aren't for everyone - especially those who are struggling or unable to conceive (my heart goes out to anyone dealing with that).
Tuesday, 2/27 - Pre-Induction
Our story starts out on Tuesday morning. I had been having pain in my knee since Sunday evening and by Tuesday morning it was super swollen.
 |
| You can see how swollen the left knee is compared to my right knee |
I'm no stranger to flares, but I usually get them in smaller joints like my fingers, wrists, or elbows. Getting one in my knee was not something I was used to so we decided to call my OB on Tuesday morning just to make sure it wasn't a blood clot. When you get a blood clot, there is swelling and it's warm to the touch - the same symptoms as a flare. My OB decided to admit me to the hospital since my induction was scheduled for the next morning. That way they could do an ultrasound on my knee to rule out a clot and keep an extra close eye on me.
Phil had already gone to work by the time my OB's nurse called back, so I rushed around the house to get what I needed for my hospital stay. My hospital bag was packed but we were expecting to go to the hospital at 7am on Wednesday so I was not prepared to leave on Tuesday morning!
When I got to the hospital, the nurse examined my knee and said she didn't think it was a clot based the feel of the fluid in my knee, but they did an ultrasound and then I settled into my room in labor and delivery.
In hindsight, it was probably better that I got admitted on Tuesday because then they were able to transition me to the blood thinner IV (which took 3 attempts to place - ouch!) and I got my consults done with hematology, the OB, the perinatalogist and the anesthesiologist. The consult with anesthesia was the hardest. My OB had thought that I would be able to get an epidural during the induction but it turns out that there is not much data about administering epidurals to someone with a blood clot that is on a higher dose of blood thinners. It increases the chance of a spinal bleed which could result in paralysis. The anesthesiologist was so kind about everything. She reviewed our options after which I said - "Maybe I should just plan on not getting an epidural" and she said that if she was me, she would not get an epidural. I also was able to text my cousin who is a nurse anesthetist to get her opinion and she concurred with the anesthesiologist. My OB came by around 8:30 that night and agreed that an epidural was off the table. We talked about my other options - nitrous oxide and fetanyl - and she reassured me that we'd get through it. Previously I hadn't planned on getting an epidural but I had been open to it when I found out I was getting induced as inductions can be longer and harder labors. So I was pretty upset on Tuesday and cried quite a bit out of fear and anxiety about what was to come. Talking with my OB helped, though, and by the time I went to bed on Tuesday night I was feeling more calm about everything.
Wednesday, 2/28 - Induction Begins
I started the day with a cervical check that showed I was a 'roomy' 1cm and 70% effaced. That was an improvement from the day before so the nurse was optimistic that the induction would take. They placed the cervidil around 8am, which is a gel that is used to ripen the cervix. It needed to stay in for 12 hours so we spent the day reading, playing cribbage (Phil beat me all 3 games - what a stinker), and we watched the monitor for contractions. I had to be continuously monitored because if the baby was under any distress, they needed to stop the induction and stop my blood thinners so they could do a spinal block for a C-section once my labs showed that my blood wasn't too thin.
 |
| Playing the waiting game |
 |
| Watching contractions come and go |
I started to get crampy by early afternoon and started to have some mild contractions. By the late afternoon they were coming regularly so we knew my body was starting to do it's thing.
 |
| My contractions are on the top. The monitor below me is the contractions of a woman who was pushing. I so badly wanted to change places with her at this point as I was ready to be done! |
The nurse took the cervadil out at 8pm and did another cervical check. Unfortunately I was only at 2cm. But after consulting with my OB, they decided to start the pitocin. Usually they would do something else to increase dilation but they wanted to get the pitocin started so they could see how the baby tolerated it. If the baby didn't tolerate it, they would stop everything and do a C-section the following day.
However, by the time they were getting ready to start the pitocin, my contractions were coming pretty regularly so they decided to hold off as they didn't want things to progress too quickly. During this part I hung out in bed and was able to breath through contractions. Phil laid down for awhile as we knew we had a long night ahead of us. I think they put the pitocin at the lowest level around midnight, though. I was able to sleep from 1:30-3 am but when I woke up the contractions were petering out so they increase my pitocin dose to see if they could get things progressing.
At that point I started to have some really painful contractions. I got Phil up and sat on the birth ball. I would sort of moan through the contractions while he rubbed my neck and shoulders and told me I could do this. The nurse could see that the contractions were more intense and asked if I wanted to start the nitrous oxide. I didn't want to start pain meds too soon, so she decided to check me around 4am to see where I was at. I was at 5cm! We were really happy about the progress I had made so she got the nitrous oxide set up. It really took the edge off the contractions at that point and I was able to lay on my side in bed during the contractions which was much more restful.
The intensity of the contractions continued to pick up so she checked me again at 5 and I was at 6cm. She consulted with my OB - who was on call that day! - and they decided to turn off my blood thinners as they thought we might have a baby in the next 5 hours or so. My OB came in and checked me around 7, I think, and I was at a 7cm so things were moving along. Once I got to this stage of labor, the nitrous oxide really didn't help much. If anything, it was sort of meditative to breath in and out of the mask but I was in a lot of pain during each contraction.
Things kind of get blurry after this but I know that the OB did another check and I was at 8 cm and then 9cm at the next couple of checks but the head had not descended. And then an hour later I was still at 9cm so she decided to break my water to see if that would get the baby to descend. When she broke my water, there was meconium in it so we knew that the baby might be distressed and not tolerate the increasing intensity of my contractions.
An hour after she broke my water, she came back and checked me again and I had made no further progress. At this point, I was so exhausted. I had only gotten 4.5 hours of sleep on Tuesday night due to getting to bed late after getting my blood thinner drip started and a middle-of-the-night blood draw to check my clotting levels. And then I had gotten 1.5 hours of sleep on Wednesday night since I was in labor. So I was exhausted and the pain from the contractions was so bad.
My OB gave us 2 options around 11:30 am (I think). I'd had a blood draw done that morning that showed that my blood clotting was at a safe level for a spinal block or epidural. So she said we could administer an epidural and see if that got my body to relax enough to let the baby descend so I could start pushing. The other option was to do a C-section. All along I wanted to avoid a C-section but at this point I was so exhausted and I knew that I did not have it in me to potentially work through more contractions and then push - potentially for hours. I was really emotional at this point and started to sob and said I felt like a wimp. My OB, who I love and trust, told me that I had been so strong and that I had given it my all. And the nurse echoed what she said. Phil also told me that this was the right decision and that I had been a warrior. So we decided to go with a C-section.
Shortly there after, I got 2 really strong back-to-back contractions and the baby's heart rate decelerated. My OB was still in the room at this point and she said that we just got confirmation that we made the right choice because if we had decided to go the epidural route, that plan was no longer an option because we needed to get the baby out. They had me switch back and forth between oxygen and the nitrous oxide to see if we could get the baby's heart rate up and I had to get on my hands and knees to see if the baby would do better in that position. This was the most vulnerable and upset I have ever been in my life. I was crying so hard and writhing in pain but Phil was amazing through all of this (even though I know he was terrified and had the hardest time seeing me in that condition).
Things moved really fast after that. They pushed off a scheduled C-section and got us into the operating room ASAP. Everyone was so incredibly nice and it was wonderful that my OB was the one doing my C-section. I have such an excellent relationship with her, so it was reassuring to have her talk me through everything. I got my spinal block and then Phil came in and sat by me and reassured me that everything was going to be ok.
It felt like it took forever for them to get the baby out but Phil said it actually happened pretty quickly. He was able to announce the gender and I'll never forget the look on his face and the emotion in his voice when he told me we had a baby boy. He cried right away when they got him out so we knew that he probably hadn't inhaled meconium and would be just fine.
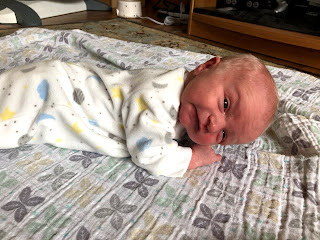
 |
| My doctor showing me baby Paul |
Phil got to cut the umbilical cord
And then they brought him over to my chest for our first family photo.
As I mentioned in my last post, I was able to do skin-to-skin with him while they stitched me up, which was incredible and so calming for both of us.
After that, I was out of the OR and in the recovery room where we did more skin to skin and tried to start breastfeeding (which didn't go all that great - breastfeeding has been a struggle but we have made so much progress thanks to meeting with lactation consultants each day we were in the hospital).

By the time we got up to our post-partum room, my parents were there and ready to meet little Paul. They ended up being our only visitors in the hospital as I was very overwhelmed by all the people in and out of our room and I spent so much of my time in the hospital topless so we could do skin-to-skin and work on breastfeeding. Luckily my family understood and will meet him later this week when we are more settled in at home. We got discharged yesterday afternoon, so I ended up being in the hospital for a week total! It's so good to be in the comfort of our home, but I am thankful for the excellent care we received while in the hospital. The nurses and lactation consultants are angels on earth.
So there's my LONG story of little Paul's arrival. Like this pregnancy, his arrival did not go how I wanted it to go. But I knew all along that it was out of my control. We are exhausted and sleep-deprived but the baby cuddles are so amazing. We keep looking at him with wonder over the fact that Phil and I created him. It's also been amazing to watch Phil become a dad. C-section recovery is SO HARD so I rely on him so much. He had to do all the diaper changes for the first several days and has just been an all-around trooper. I didn't think I could love him more than I already did, but I do.